Understanding the impact of Spina Bifida on bladder function is fundamental for developing effective management strategies tailored to individual needs.
Spina Bifida, a congenital condition characterized by the incomplete closure of the spinal column, can profoundly influence an individual’s bladder control and overall urinary function. This condition arises during foetal development, leading to varying degrees of neurological impairment that can affect the spinal cord and associated nerve pathways. In many instances, individuals with Spina Bifida experience neurogenic bladder, a condition where the nerves that control bladder function are damaged or non-functional, resulting in altered bladder sensation and control.
The severity of bladder dysfunction may vary significantly among those who have Spina Bifida, depending primarily on the level and extent of spinal cord involvement. Some individuals may experience a flaccid bladder, which is unable to contract effectively, leading to urinary retention. Conversely, others may experience an overactive bladder, characterised by frequent or involuntary contractions that result in urgency and incontinence. These physiological challenges necessitate tailored bladder management strategies to ensure a high quality of life and minimise complications such as urinary tract infections (UTIs) and kidney damage.
Effective bladder management is crucial for individuals with Spina Bifida. One common approach to maintaining greater control over their urinary health is Clean Intermittent Self-Catheterization.
What is Clean Intermittent Self-Catheterization (CISC)?
Clean Intermittent Self-Catheterization (CISC), Intermittent Self-Catheterization (ISC) or Clean Intermittent Catheterization (CIC) is a medical procedure that involves the periodic insertion of a catheter into the bladder to evacuate urine. This practice is especially relevant for individuals with Spina Bifida, a condition that often leads to bladder dysfunction due to nerve damage called neurogenic bladder. The primary goal of Clean Intermittent Self-Catheterization (CISC) is to improve bladder management, ensuring that the bladder is emptied regularly and effectively to avoid complications associated with urinary retention.
What are the benefits of Clean Intermittent Self-Catheterization (CISC)?
The benefits of Clean Intermittent Self-Catheterization (CISC) are multi-faceted. Firstly, CISC enhances bladder control, reducing the risk of urinary tract infections (UTIs) and other complications, such as bladder stones and renal impairment. CISC prevents Vesicoureteral reflux, preventing the backflow of urine that could damage the kidneys. Regular emptying of the bladder helps manage urinary storage and voiding at will, which is crucial for individuals who can’t urinate by themselves. Moreover, this method promotes better hygiene and reduces the occurrence of incontinence episodes, ultimately leading to an improved quality of life, supporting your social and love life, and promoting sexual health.
Furthermore, Clean Intermittent Self-Catheterization empowers individuals with Spina Bifida by providing them with autonomy over their bladder health. When SB individuals learn to perform self-catheterization independently, they gain confidence and a sense of control, enabling enhanced participation in daily activities. Our education surrounding CISC also includes instruction on proper techniques, hygiene practices, and the choice of appropriate catheters, which contributes to the overall effectiveness of the procedure.
Additionally, the relevance of CISC extends to its role in long-term health management. By adopting the Clean Intermittent Self-Catheterization practice, individuals can establish a sustainable routine that supports their bladder health, ultimately lessening the impact of Spina Bifida on their daily lives. In short, understanding the fundamentals of Clean Intermittent Self-Catheterization is crucial for individuals with Spina Bifida, as it lays the groundwork for effective bladder management and enhances overall well-being.
Post-Catheterization Care and Maintenance
After self-catheterization, proper post self-catheterization care is essential to ensure urinary health and the effectiveness of this procedure.
Verifying Proper Bladder Emptying
Verifying proper bladder emptying is a crucial part of post-catheterization care. After the self-catheterization process, individuals should monitor for signs of complete bladder emptying, which means post-void residual volume should be less than 50 ml. There are a couple of ways you can do so:
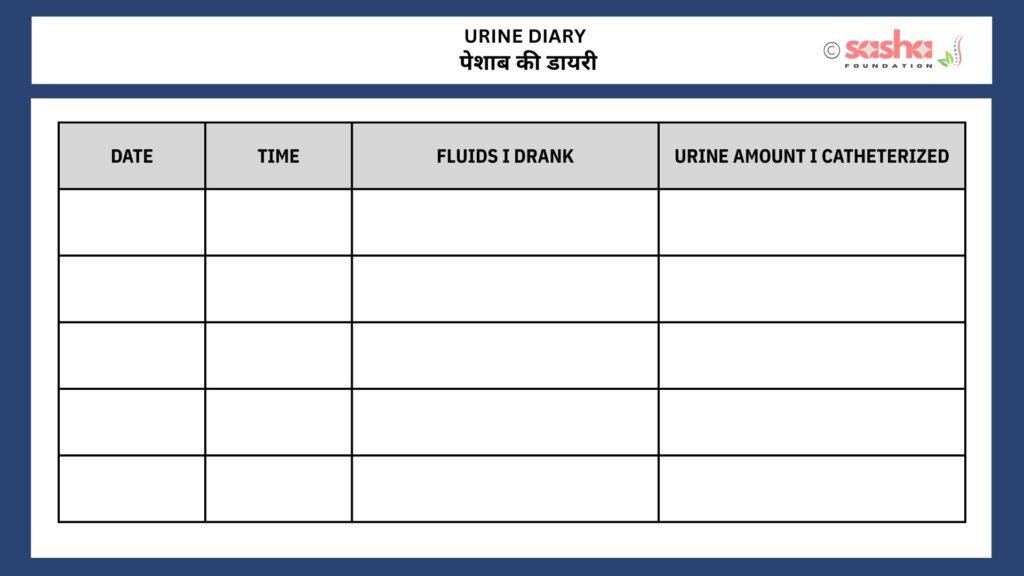
Maintaining a urine diary
We suggest this when someone is just starting catheterization or has been catheterising for a long time but is seeing signs like an increase in catheterization frequency, urine incontinence (leakage) or both.
A urine diary involves meticulously tracking your daily liquid intake and urine output, including the timing for each. For the intake, you record the quantity and type of fluids consumed—such as water, milk, juice, tea, or coffee—along with the exact times. For the output, you note what time you catheterised and the voided urine volume. By comparing your fluid intake to urine output, you can better understand when your bladder feels full and identify the leakage patterns. With this information, you can have an informed discussion with your doctor. This verification helps in identifying potential complications early, including urinary retention or incomplete catheterization. Get in touch with Sasha if you want to learn more about this.
Use this chart as a sample to make your own record book. This will help you adjust your catheterization times.
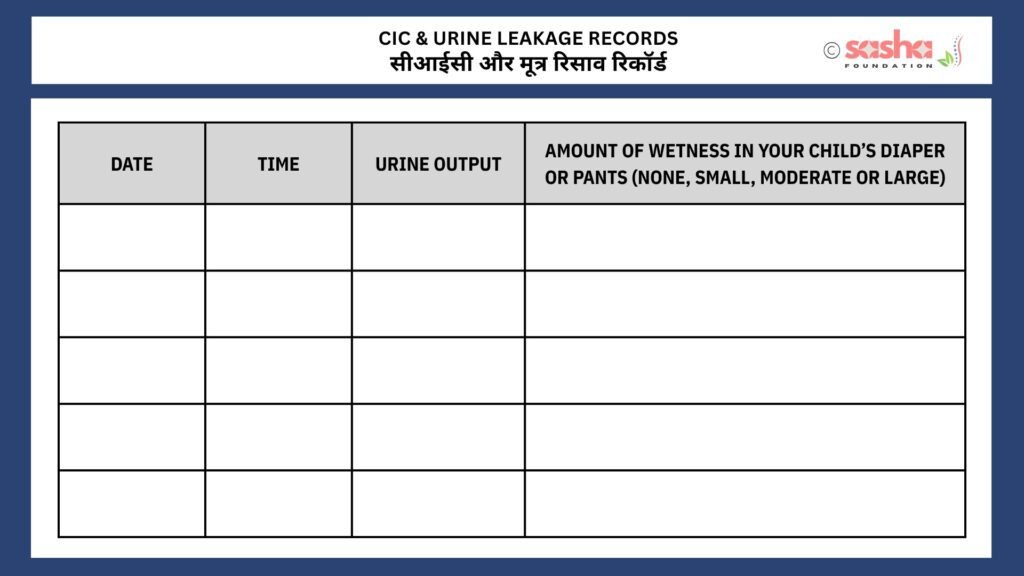
Use this form to write down the date, time and urine output each time your child does CIC. Also, record the urine leakage.
KUB ultrasound
A kidney and urinary bladder ultrasound (sonography), performed both before and after voiding (post-catheterization), is an effective method to detect complications or incomplete catheterization. It is considered the most reliable test for estimating residual urine volume, with a residual volume of less than 50 ml being regarded as normal.
For those new to catheterization, undergoing an ultrasound is generally recommended to ensure proper management and identify any potential issues early on. Individuals with long-term catheterization experience who are not experiencing any bladder-related problems may consider having an annual ultrasound for routine monitoring.
Awareness of potential complications is vital for ongoing bladder health management. Signs to monitor include discomfort or pain, urination urgency shortly after catheterization, or any unusual changes.
Emotional and Psychological Aspects of Self-Catheterization
Learning self-catheterization can bring a unique set of emotional and psychological challenges, particularly for individuals with Spina Bifida. This process may evoke feelings of anxiety, embarrassment, or frustration, as it often involves adjusting to a new routine that is critical for maintaining independence and health. The emotional response to self-catheterization may differ from person to person; however, it is important to acknowledge these feelings and address them constructively.
One of the most effective coping strategies is to seek support from others who understand the process. This support can come from healthcare professionals, family members, or Sasha’s support groups, comprised of individuals with similar experiences. Engaging in open discussions about the challenges of self-catheterization can help overcome apprehension and foster a sense of community. At Sasha, we offer invaluable insights into practical strategies for overcoming obstacles.
Maintaining a positive outlook throughout the self-catheterization process is also essential. Relaxation techniques, such as mindfulness or deep-breathing exercises, can alleviate stress associated with the initial learning period.
Lastly, it is crucial to remember that self-catheterization is a skill that can be mastered over time. Celebrating small milestones can significantly impact one’s emotional well-being and self-esteem. In time, individuals may find themselves more comfortable with the process, leading to increased confidence and independence. Thus, embracing both the challenges and rewards of self-catheterization can contribute to a positive, empowering journey toward self-management and autonomy.
Please Note
The information provided on our website is not intended as medical advice for any individual. Since specific cases may differ from the general information presented, SASHA recommends consulting a qualified medical or other professional for personalized advice.
About the Author
Raul/DJ Vivek
Meet Vivek Bharadwaj, a remarkable individual who has defied the odds and soared to new heights despite living with Spina Bifida. As the founder of the Sasha Foundation, Vivek tirelessly advocates for others facing similar challenges. His unwavering commitment to support, awareness, and empowerment had made a lasting impact on the Spina Bifida community.





Leave a Reply
You must be logged in to post a comment.